sudden vision loss in one or both eyes
sudden vision loss is one of the eye disorders considered critical in the field of ophthalmology due to its potential severity. The causes of sudden vision loss in one or both eyes can vary, making it a significant condition that, if not addressed promptly, can lead to serious eye damage and even result in complete blindness.
If you experience sudden vision loss, it is crucial to contact emergency services immediately. Seek the expertise of an ophthalmologist or treating physician promptly, as there is a short window for diagnosis and treatment. Do not wait to see if it resolves on its own. In the case of partial vision loss, migraines are the most probable cause, but there are certainly other reasons as well.
complete or partial sudden vision loss
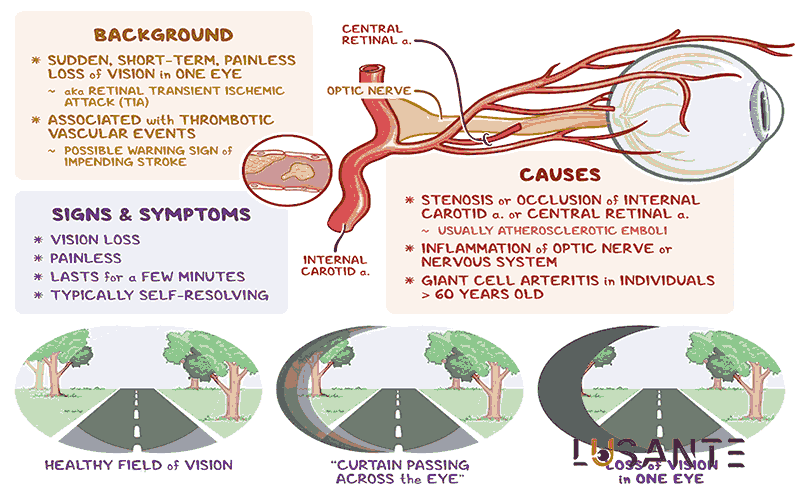
This can occur when there is a blockage in your retinal artery, referred to by the doctor as either central retinal artery occlusion or branch retinal artery occlusion. It also signals a risk of a stroke or heart attack. Blood clotting and the blockage of blood vessels in the eye can occur similarly to the situation where a plaque breaks off in coronary arteries, leading to a blood clot and a subsequent heart attack. If this event occurs in your brain, it results in an ischemic stroke caused by blood clot formation.
Clots can induce temporary blindness in one eye, typically lasting 20 to 30 minutes, often resembling the descent of a dark curtain. Doctors term this condition amaurosis fugax. Without prompt treatment, this blockage can lead to permanent blindness. Your doctor may prescribe medication to dissolve the clot, and in some cases, angioplasty, a method to open blocked blood vessels, may be necessary. Moreover, it can serve as a warning sign for reducing the risk of a heart attack or stroke.

Causes of sudden vision loss
sudden vision loss; Migraine
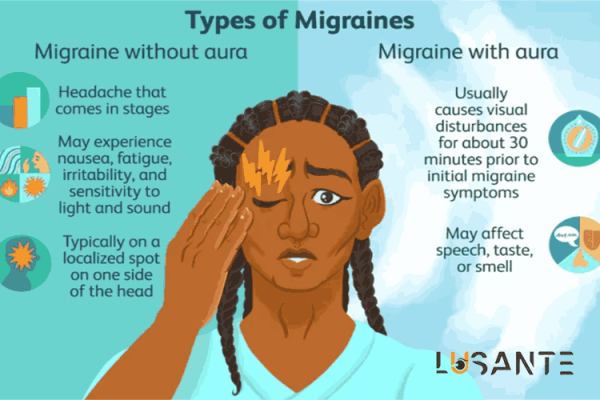
Migraine currently stands as the most prevalent cause of partial vision loss. During a migraine episode, halos may appear in the eyes, affecting vision in both eyes. Observable phenomena include blinking lights, shimmering spots, or blind spots.
In the case of retinal migraine, only one eye is affected. This rare condition can lead to partial or total blindness for a brief period, usually lasting 10 to 20 minutes, typically occurring before or during a headache.
Migraines often present visual symptoms referred to as migraine auras. Common visual manifestations include areas that a person cannot see clearly. Approximately 25 to 30 percent of people with migraines experience visual aura symptoms, which can occur with or without a headache.
Typical visual disturbances during a migraine include:
- Zigzag lines
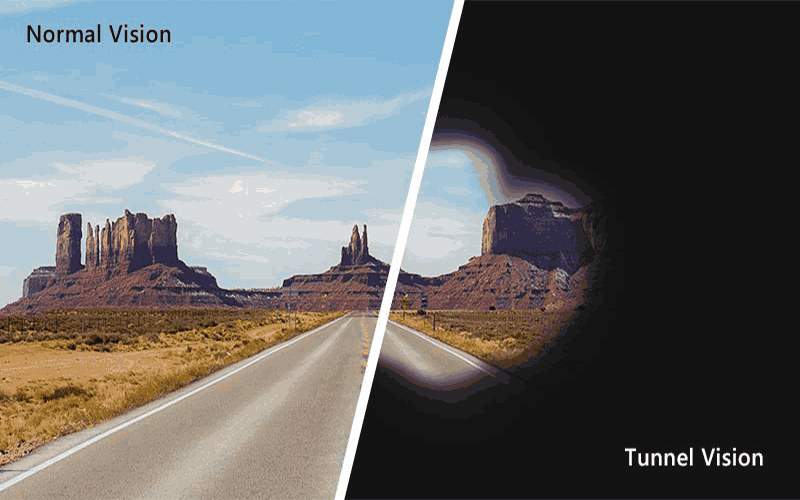
- Tunnel vision
- Loss of vision to the left or right
- Complete loss of vision
Migraine auras usually endure for 10 to 30 minutes, or less than an hour, though some may last only a few seconds. Managing symptoms involves avoiding bright lights, loud noises, and taking migraine medications.
Related Article: Peripheral Vision Loss and Tunnel Vision
sudden vision loss; Retinal Vasospasm
Similar to migraines, this condition can cause temporary vision loss, and effective treatment can fully restore your vision. When a blood vessel in your retina tightens, it triggers retinal vasospasm, leading to reduced blood flow and temporary vision loss in one eye.
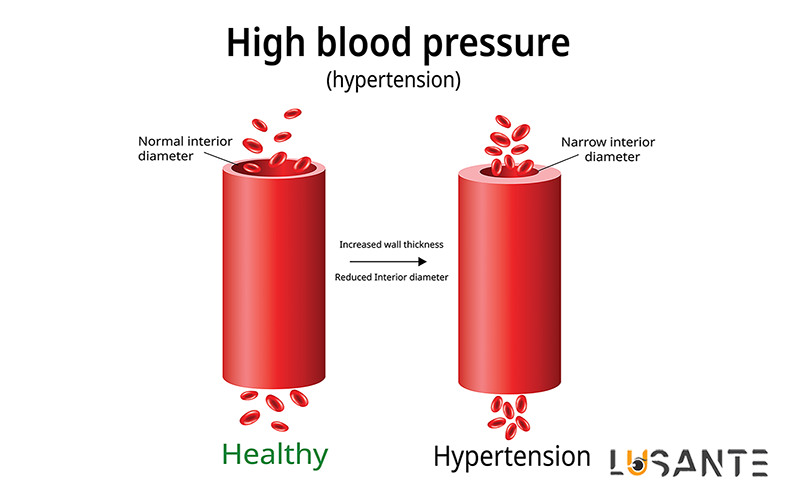
Various factors can contribute to vasospasm, including retinal migraines, atherosclerosis, and high blood pressure. If you experience retinal vasospasm, your doctor may recommend aspirin or a type of medication called a calcium channel blocker to alleviate it. Collaborating with your doctor will help identify the underlying cause of retinal vasospasm.
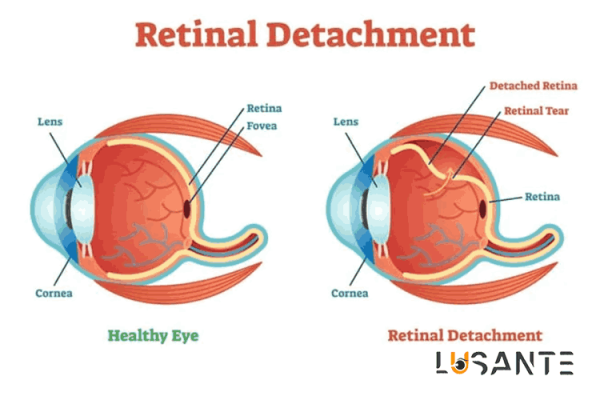
On the other hand, a detached retina occurs when the retina lifts off the back of the eye, potentially causing partial or complete vision loss in the affected eye. When someone has a detached retina, it may feel like something is blocking part of their vision. Retinal detachment is a severe condition, and without timely treatment, it can lead to permanent vision loss. Treatment typically involves a surgical procedure determined by the doctor’s assessment.
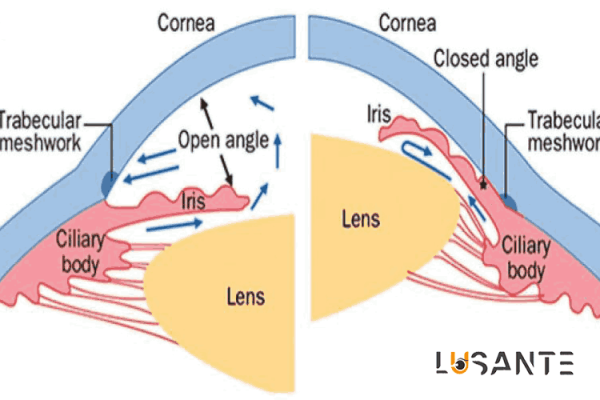
sudden vision loss; Angle-Closure Glaucoma and Vision Loss
When the iris of your eye enlarges, it can obstruct proper fluid drainage, leading to increased pressure in your eye. This may cause discomfort, short-term blurred vision, nausea, halos, or blindness in one eye. Medications, such as eye drops or oral tablets like prostaglandins or beta-blockers, can help alleviate eye pressure. If these measures prove ineffective, a procedure called iridotomy may be necessary. In this surgery, a small hole is created in your iris to facilitate fluid drainage and reduce pressure.
The term “glaucoma” encompasses a group of diseases that can damage the optic nerve at the back of the eye, potentially leading to vision loss and blindness. Symptoms of glaucoma can manifest so gradually that an individual may not realize they have the condition until an eye examination is conducted. Those with glaucoma may experience a slow loss of vision, often starting peripherally and affecting one or both eyes.
In cases of angle-closure glaucoma, eye pressure can rapidly rise, causing pain, nausea, vomiting, or vision loss. Healthcare professionals usually manage this condition with eye drops, though laser treatment or surgery may be necessary at times. If left untreated, glaucoma can ultimately lead to blindness.
Prescribed eye drops serve as the primary treatment for glaucoma. While these drops can reduce eye pressure and prevent further damage to the optic nerve, they cannot reverse damage that has already occurred.
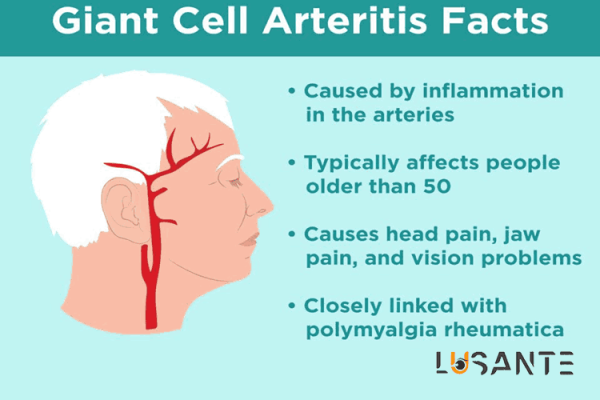
sudden vision loss; Giant Cell Arteritis
This condition is uncommon but constitutes a significant cause of vision loss in individuals over 50 years old, leading to inflammation in the arteries, especially those around the head. Symptoms encompass headache, scalp sensitivity, jaw pain, fever, and fatigue.
Giant Cell Arteritis typically results in sudden vision loss in one eye, and without treatment, it can lead to permanent blindness within one or two weeks. Your doctor will likely initiate treatment with a corticosteroid medication such as prednisone. Although you may experience improvement within a few days, it may be necessary to continue the medication for 1 or 2 years. Tocilizumab, a medication, has also been approved to assist in treating Giant Cell Arteritis.
Rheumatoid Arteritis is a condition characterized by severe and often intense headaches, typically affecting both temples. The headache may gradually worsen, come and go, or temporarily subside.
In general, symptoms of Giant Cell Arteritis include:
- Severe and persistent headache, usually in the temple area
- Scalp tenderness
- Jaw pain when chewing or opening the mouth
- Fever
- Fatigue
- Unintended weight loss
- Sudden and permanent loss of vision or double vision, especially in individuals with jaw pain.
Pain and stiffness in the neck, shoulders, or hips are common symptoms of an associated disorder, Polymyalgia Rheumatica, with approximately 50% of individuals with Giant Cell Arteritis also having Polymyalgia Rheumatica.
sudden vision loss; Retinal Disorders
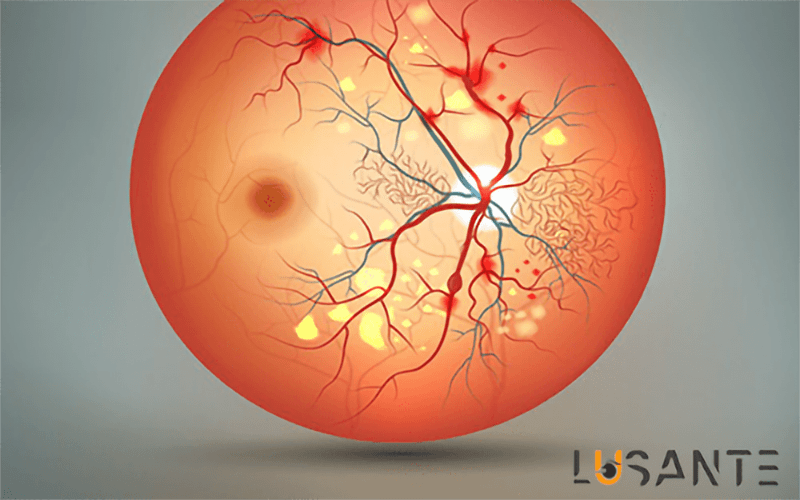
The retina, a complex and delicate tissue lining the inner surface of the eye, plays a pivotal role in the process of vision. Various retinal disorders can compromise this essential structure, leading to a range of visual impairments.
Related Article: Retinal Vascular Disorders
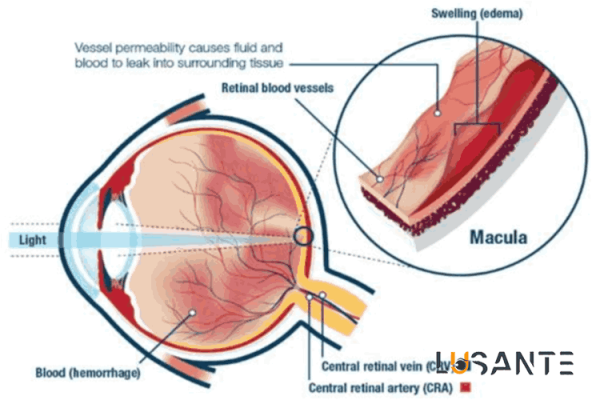
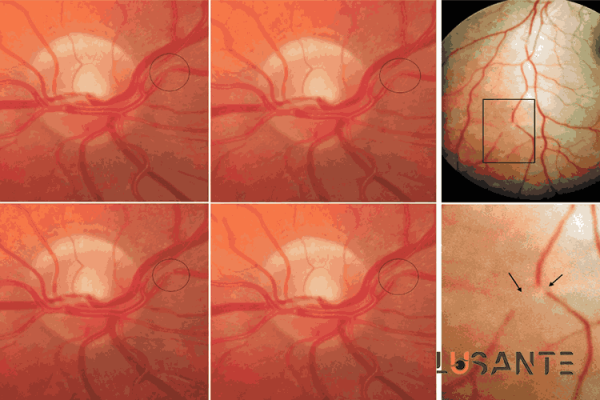
The central retinal artery occlusion (CRAO) stands as a formidable retinal disorder characterized by the sudden blockage of the central retinal artery. This critical vessel, responsible for supplying oxygen and nutrients to the inner layers of the retina, can face obstruction due to emboli or thrombosis, resulting in rapid and profound vision loss. CRAO is a serious condition associated with sudden vision loss.
In contrast, central retinal vein occlusion (CRVO) involves the obstruction of the central retinal vein, leading to impaired venous outflow and retinal congestion. This disorder can manifest as sudden or gradual vision loss, often accompanied by retinal hemorrhages and macular edema. CRVO is a significant contributor to sudden vision loss in affected individuals
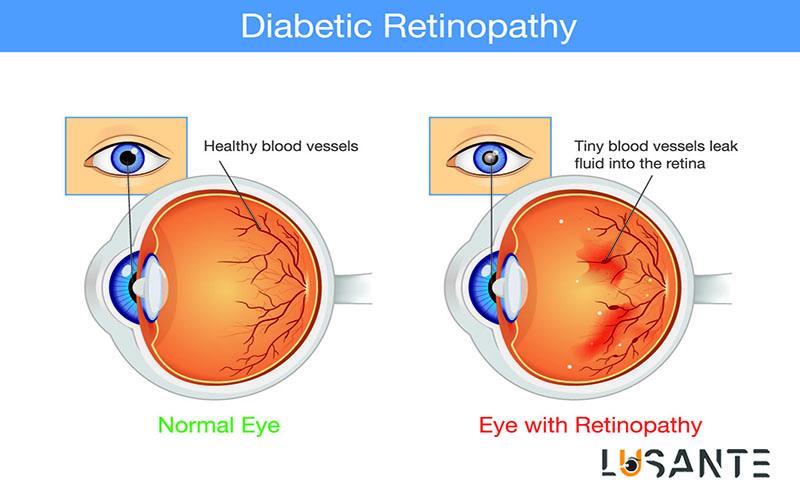
Diabetic retinopathy, a common complication of diabetes mellitus, affects the microvasculature of the retina. Chronic hyperglycemia induces vascular changes, potentially causing vision loss due to macular edema or vitreous hemorrhage. Diabetic retinopathy poses a risk of sudden vision loss, emphasizing the need for proactive management.
Related Article: Which Supplement Helps to Prevent Diabetes And Vision loss? | 5 Certain Method To Reduce
Another prevalent retinal disorder is age-related macular degeneration (AMD), involving the degeneration of the macula crucial for sharp, central vision. The two main types, dry and wet AMD, feature the accumulation of drusen or abnormal blood vessels, respectively, leading to varying degrees of vision impairment. AMD can contribute to gradual or sudden vision loss.
Related Article: 8 Amazing ways to Prevent Age Related Macular Degeneration
Retinal detachment is a serious condition where the retina peels away from the underlying tissue, disrupting the normal flow of visual signals. This separation can cause flashes of light, floaters, and, if untreated, permanent vision loss. Trauma, age-related changes, or underlying retinal diseases can contribute to retinal detachment, leading to sudden vision loss.
Retinitis pigmentosa, a group of inherited retinal disorders, involves the progressive degeneration of photoreceptor cells. This leads to peripheral vision loss, night blindness, and, in advanced stages, central vision impairment. Genetic factors play a crucial role in the development of this disorder, potentially resulting in sudden vision loss.
Retinal artery macroaneurysm is characterized by localized dilation and potential rupture of a retinal artery. This condition can result in hemorrhage and compromise blood flow to surrounding retinal tissue, causing vision disturbances. Hypertension is a common risk factor for the development of retinal artery macroaneurysms, emphasizing the link between hypertension and sudden vision loss.
retinal disorders encompass a diverse array of conditions, each with unique characteristics and implications for visual health. The understanding of these disorders continues to evolve, driven by advancements in diagnostic technologies and therapeutic modalities. A comprehensive approach to their diagnosis and management is crucial for preserving vision and improving outcomes for individuals affected by these conditions, especially those at risk of sudden vision loss.
sudden vision loss; Optic Nerve Disorders
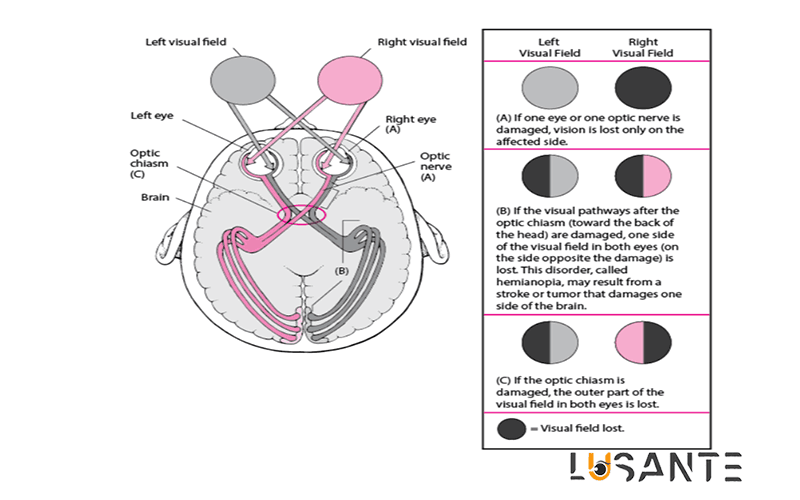
The optic nerve, a fundamental component of the visual system, serves as the conduit for transmitting visual information from the eyes to the brain. Disorders affecting the optic nerve constitute a diverse spectrum of conditions, each presenting unique challenges in terms of diagnosis and management. This comprehensive exploration aims to shed light on the intricacies of optic nerve disorders, encompassing their anatomy, clinical manifestations, diagnostic approaches, and the complexities inherent in their treatment.
The optic nerve, arising from the optic disc at the back of each eye, carries vital visual stimuli to the brain. This intricate pathway involves the optic chiasm and optic tracts, forming an essential link in the complex network of vision. Understanding the anatomy is fundamental to grasping the nuances of optic nerve disorders.
Optic nerve disorders manifest through a myriad of symptoms, ranging from sudden vision loss and pain with eye movement to color vision impairment. The clinical presentation is diverse and varies significantly based on the underlying cause, which may include ischemic conditions, inflammation, compressive lesions, hereditary factors, or traumatic injuries.
Ischemic optic neuropathy is characterized by an insufficient blood supply to the optic nerve, leading to sudden vision loss. The condition can manifest in arteritic forms associated with giant cell arteritis or non-arteritic forms resulting from vascular insufficiency. Recognition of this distinction is crucial for appropriate management.
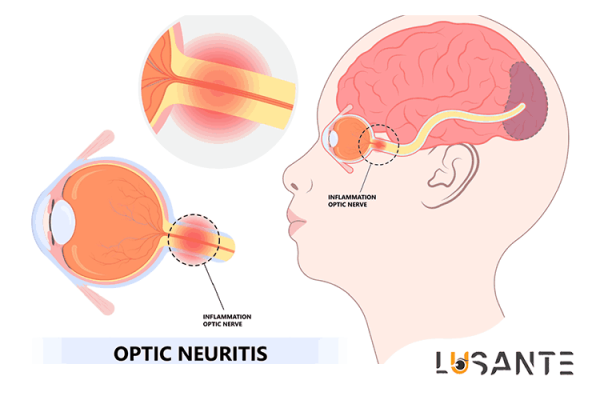
Optic neuritis, marked by inflammation of the optic nerve, is often linked to demyelinating diseases like multiple sclerosis. The sudden onset of symptoms, including vision loss and pain with eye movement, necessitates prompt intervention to mitigate potential long-term consequences.
External pressure on the optic nerve due to tumors or masses results in compressive optic neuropathy. The impact of this pressure compromises nerve function, leading to visual field defects and, if left untreated, permanent vision loss. Identifying the underlying cause is essential for effective management.
Genetic mutations contribute to hereditary optic neuropathies such as Leber’s hereditary optic neuropathy and dominant optic atrophy. These conditions present with painless, bilateral vision loss and may exhibit a variable age of onset. Genetic counseling and early detection are integral components of managing hereditary optic neuropathies.
Traumatic optic neuropathy is a consequence of head trauma or injury to the orbit. Direct or indirect damage to the optic nerve results in varying degrees of visual impairment. Prognosis is contingent upon the nature and extent of the injury, highlighting the need for personalized treatment strategies.
Accurate diagnosis of optic nerve disorders demands a comprehensive evaluation. This includes a detailed medical history, visual acuity testing, pupillary examination, and advanced imaging studies such as MRI or CT. Supplementary tests like visual field testing and optical coherence tomography contribute valuable insights into optic nerve structure and function.
Effectively managing optic nerve disorders involves addressing the root cause. Treatment strategies may encompass immunosuppressive therapy for inflammation, surgical intervention for compressive lesions, or genetic counseling for hereditary conditions. The complexity lies in the diversity of causes, necessitating tailored and individualized approaches for optimal outcomes.
sudden vision loss; Vascular Events
Vascular events affecting the visual system constitute a multifaceted realm with implications ranging from subtle visual disturbances to profound vision loss. This comprehensive exploration delves into the intricate landscape of vascular events, encompassing their diverse causes, clinical manifestations, diagnostic approaches, and the challenges encountered in their management.
Understanding the vascular anatomy of the visual system is paramount to comprehending the impact of vascular events. The intricate network of arteries and veins supplying the eyes plays a critical role in maintaining the health and function of ocular structures.
Ischemic events, characterized by inadequate blood supply to specific areas, can significantly affect visual health. Central retinal artery occlusion (CRAO) represents a severe ischemic event, often caused by emboli or thrombosis, leading to sudden and profound vision loss. On the other hand, central retinal vein occlusion (CRVO) involves impaired venous outflow, resulting in retinal congestion, hemorrhages, and potential vision impairment.
Underlying systemic conditions contribute to the occurrence of vascular events affecting the eyes. Hypertension, diabetes, and hypercoagulable states can predispose individuals to arterial or venous occlusions, disrupting the delicate balance of blood supply and drainage in the ocular structures.
Inflammatory vasculopathies pose a unique challenge in the context of vascular events. Conditions such as vasculitis can lead to inflammation of blood vessels supplying the eyes, compromising their integrity and function. The clinical manifestations can vary widely, emphasizing the need for a thorough diagnostic approach.
Vascular events often present with distinctive clinical manifestations. Sudden vision loss, visual field defects, retinal hemorrhages, and changes in the appearance of the optic disc are common features. The variability in symptoms necessitates a comprehensive evaluation to ascertain the underlying cause.
Accurate diagnosis of vascular events requires a multifaceted approach. Ophthalmic examinations, including fundoscopy and fluorescein angiography, provide insights into retinal blood flow and vascular integrity. Systemic evaluations, such as blood pressure monitoring and laboratory tests, aid in identifying predisposing factors.
Managing vascular events in the context of visual health poses challenges due to the diversity of underlying causes. Treatment strategies may involve systemic interventions, such as anticoagulation for thrombotic events or immunosuppression for inflammatory vasculopathies. Coordinating care between ophthalmologists and other specialists is crucial for comprehensive management.
The prognosis of vascular events varies based on factors such as the rapidity of intervention, the extent of ocular involvement, and the underlying systemic health of the patient. Long-term implications may include visual sequelae, the recurrence of events, or the development of secondary complications, including the risk of sudden vision loss.