All about Transient Vision Loss
Transient vision loss, often referred to as transient visual obscurations, is a temporary but concerning visual disturbance. This article delves into the causes, symptoms, and management of this condition to provide a comprehensive understanding.
What is Transient Vision Loss?
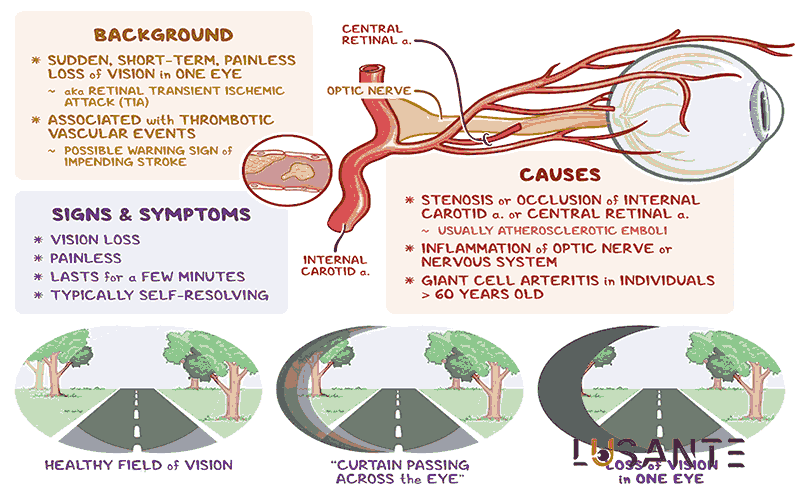
Transient vision loss is a perplexing visual phenomenon characterized by the temporary loss or impairment of vision. Transient vision loss can manifest as a sudden dimming, blurring, or complete blackout of vision, typically lasting for seconds to a few minutes. While it may be a fleeting experience, transient vision loss is a matter of concern and warrants understanding.
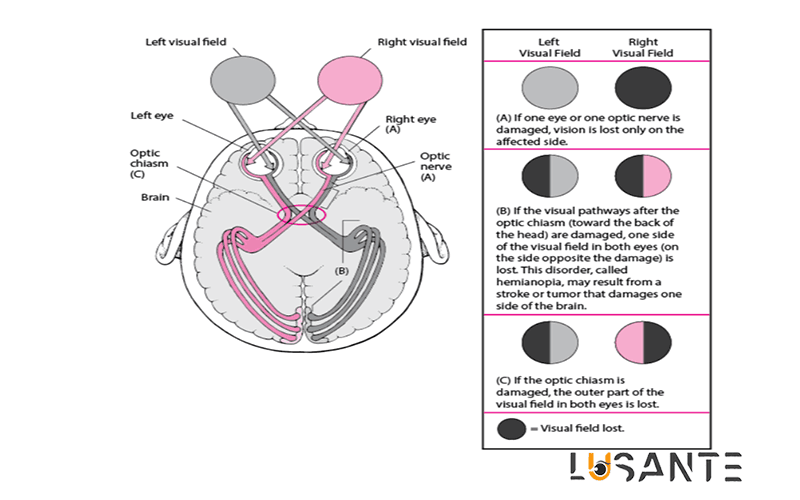
Transient vision loss often occur with no prior warning, leaving those who experience them both bewildered and anxious. These occurrences can be either unilateral, affecting one eye, or bilateral, impacting both eyes, making it a variable condition.
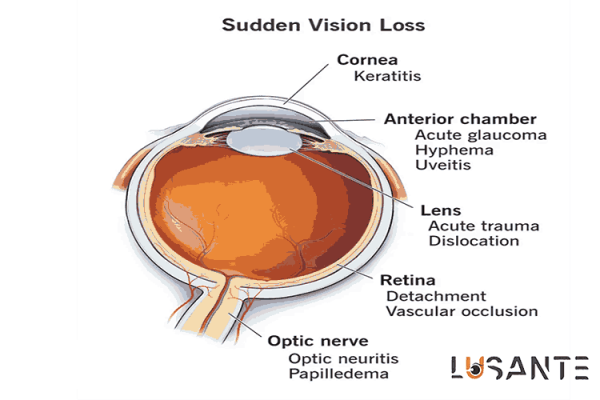
One of the most challenging aspects of transient vision loss is that it can be a sign of an underlying medical issue. The causes Transient vision loss are diverse and can be broadly categorized into vascular, neurological, and ophthalmological factors.
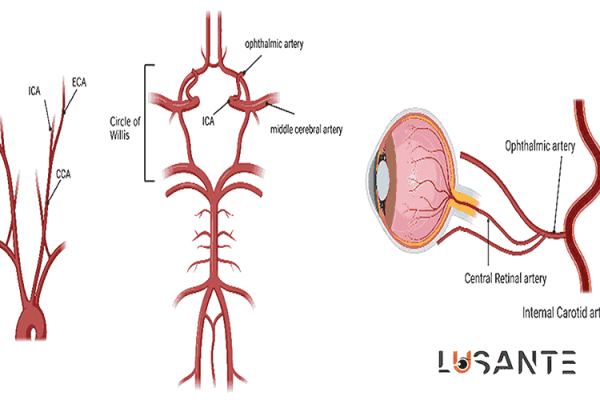
Vascular causes of transient vision loss are often linked to the eye’s blood supply. Conditions like amaurosis fugax, caused by a transient blockage of blood flow to the eye, fall under this category.
Neurological factors can also play a role. Migraines, for instance, can lead to visual disturbances, sometimes referred to as visual migraines, which may involve transient vision loss.
Ophthalmological conditions such as glaucoma, a group of eye disorders characterized by optic nerve damage, can contribute to transient vision loss. Increased pressure within the eye can impact blood flow to the optic nerve, resulting in Transient vision loss.
When an individual experiences transient vision loss, it is typically a painless occurrence. There is no discomfort or pain associated with Transient vision loss, which can sometimes make it more challenging to identify the cause.
The diagnosis of transient vision loss can be complex due to its episodic and unpredictable nature. A thorough evaluation, including a detailed medical history and various diagnostic tests, is often required to determine the underlying cause.
Treatment and management of transient vision loss depend on identifying the specific cause. Blood pressure control, antiplatelet agents, or even surgery in certain cases may be recommended.
Living with transient vision loss can be challenging, as these episodes can disrupt daily life. Coping strategies and support networks are vital for individuals dealing with this condition.
Specialized Evaluation for Transient Vision Loss
While understanding the basics of transient vision loss is essential, a more in-depth look into its specialized evaluation is warranted. When patients present with this condition, healthcare professionals must conduct a comprehensive assessment to determine the cause and formulate an appropriate management plan.
- Detailed Medical History: The foundation of diagnosing transient vision loss lies in taking a detailed medical history. Patients are asked to provide information about the frequency, duration, and nature of their episodes. Any associated symptoms or triggers, such as headaches in the case of migraines, should also be noted.
- Neurological Examination: Given the potential neurological causes of transient vision loss, a thorough neurological examination is crucial. This examination includes assessing motor and sensory function, reflexes, coordination, and cranial nerve function. Any abnormalities may indicate underlying neurological issues that need further investigation.
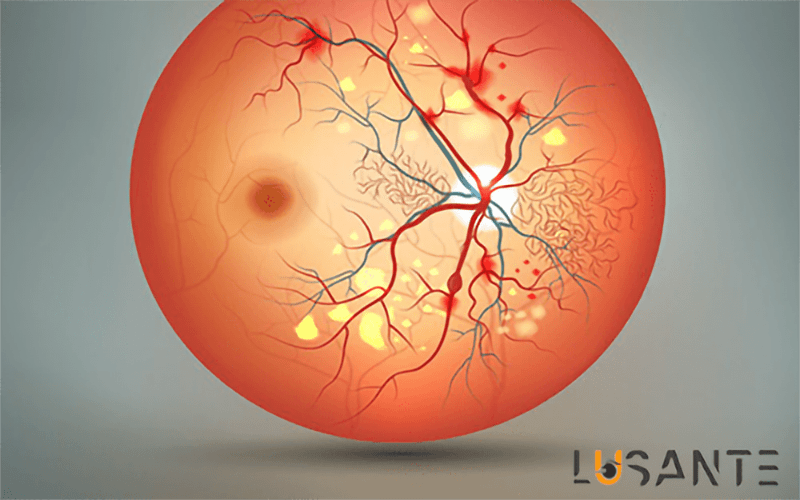
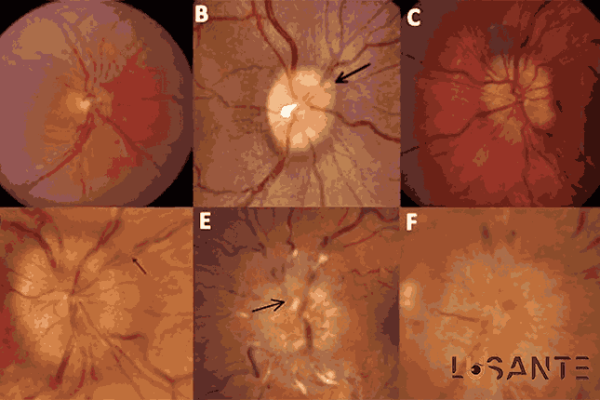
- Ophthalmological Evaluation: The eyes themselves require thorough examination. This evaluation involves assessing visual acuity, visual field testing, tonometry to measure intraocular
pressure, and fundoscopy to examine the optic nerve and retina. Any abnormalities in these assessments can provide critical clues to the cause.
- Cardiovascular Assessment: Because vascular factors are a common cause, a cardiovascular assessment is essential. This involves checking blood pressure and conducting tests such as carotid artery ultrasound to detect any plaques or stenoses that could impede blood flow to the eyes.
- Blood Tests: Blood tests are often necessary to rule out systemic conditions. These may include tests for markers of inflammation, lipid profile, blood glucose levels, and coagulation studies.
- Imaging Studies: In many cases, imaging studies are instrumental in identifying the cause of transient vision loss. Magnetic resonance imaging (MRI) of the brain and magnetic resonance angiography (MRA) of the neck vessels can reveal neurological or vascular abnormalities. In some cases, a computed tomography (CT) scan may be performed.
- Electroencephalogram (EEG): For patients with suspected neurological causes, an EEG may be conducted to record the electrical activity of the brain. This can help diagnose conditions like epilepsy, which may present with visual disturbances.
- Management Strategy Selection: Once the underlying cause is identified, the choice of management strategy depends on the specific diagnosis. For example, if the cause is atherosclerosis in the carotid arteries, management may involve antiplatelet medications, blood pressure control, and lifestyle modifications. In cases where migraines are the culprit, management could include migraine-specific medications and lifestyle adjustments.
- Patient Education: A critical aspect of managing transient vision loss is educating patients about their condition, its potential triggers, and the importance of adherence to prescribed treatments. Lifestyle modifications, including diet, exercise, and smoking cessation, may be recommended.
- Follow-Up: Patients with transient vision loss often require ongoing follow-up to monitor their condition and treatment effectiveness. Regular check-ups can help adjust the management plan as needed.

Prevalence and Risk Factors
Transient vision loss (TVL), also known as transient visual obscurations (TVO), is a clinical phenomenon characterized by temporary, partial, or complete loss of vision in one or both eyes. This condition can be a source of concern for both patients and healthcare professionals, as it may be a harbinger of more serious underlying conditions. Further in the article, we will explore the prevalence and risk factors associated with transient vision loss.
Transient Vision Loss: Prevalence
The prevalence of TVL is challenging to estimate precisely due to its transient and often self-resolving nature. However, it is not an uncommon complaint in clinical practice, and its incidence tends to increase with age. A rough estimate suggests that approximately 1 in 200 adults may experience TVL during their lifetime. The condition may also be underreported as some individuals may not seek medical attention for transient episodes, especially if they resolve spontaneously.
Transient Vision Loss: Risk Factors
- Papilledema
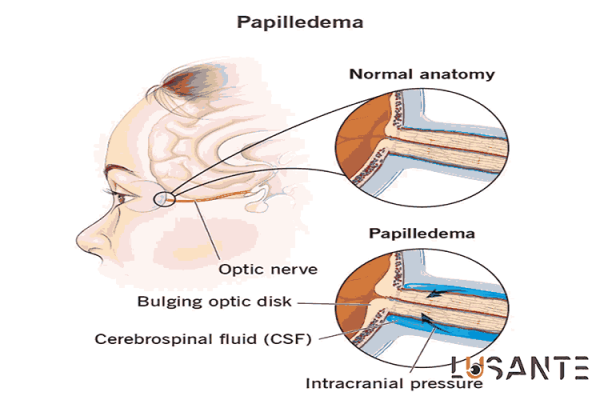
Papilledema is a medical condition that refers to the swelling of the optic disc, the point where the optic nerve enters the eye. This condition is often a sign of increased intracranial pressure, which can be caused by various underlying health issues. Understanding papilledema is crucial because it is not a disease in itself but rather a manifestation of an underlying problem that requires medical attention.
Causes of Papilledema
Papilledema primarily occurs due to increased pressure within the skull, a condition known as intracranial hypertension. Some common causes of papilledema include:
- Idiopathic Intracranial Hypertension (IIH): This is a condition characterized by elevated intracranial pressure of unknown cause, predominantly affecting obese women of childbearing age. IIH can lead to papilledema and, if left untreated, potentially cause vision loss.
- Space-Occupying Lesions: Tumors, cysts, or abscesses within the brain can exert pressure on surrounding tissues, leading to increased intracranial pressure and papilledema.
- Cerebral Edema: Swelling of the brain tissue due to various factors, such as trauma, infection, or vascular disorders, can result in elevated pressure and papilledema.
- Hydrocephalus: A buildup of cerebrospinal fluid in the brain’s ventricles can lead to increased intracranial pressure and, subsequently, papilledema.
- Subarachnoid Hemorrhage: Bleeding in the space surrounding the brain, often caused by an aneurysm rupture, can result in papilledema.
Symptoms of Papilledema
The most common symptom of papilledema is bilateral optic disc swelling. Other signs and symptoms may include:
- Blurred Vision: As the swelling affects the optic nerve, it can lead to blurry or distorted vision.
- Headaches: People with papilledema often experience severe headaches, particularly in the morning.
- Nausea and Vomiting: These symptoms can be associated with the increased intracranial pressure.
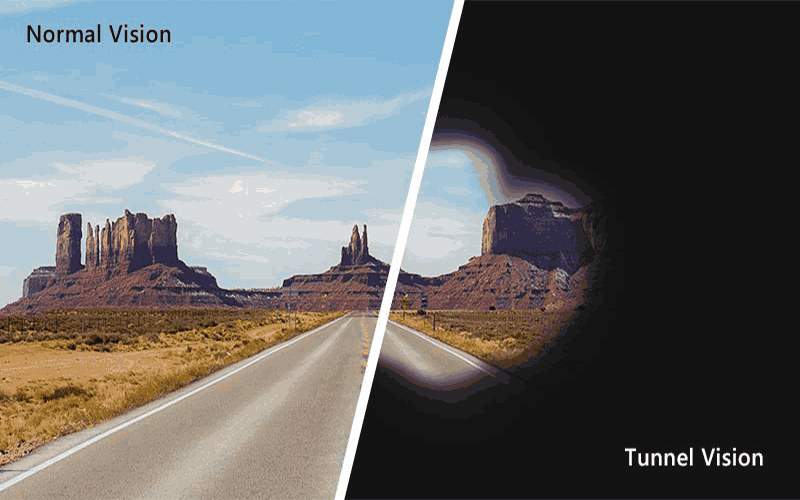
- Visual Disturbances: Changes in vision, such as blind spots, reduced peripheral vision, or seeing “halos” around lights, may occur.
Diagnosis of Papilledema
Diagnosing papilledema involves a comprehensive eye examination and often requires additional tests and imaging to determine the underlying cause. Ophthalmoscopy, which involves examining the optic disc through a dilated pupil, is a key diagnostic tool. Imaging studies like MRI or CT scans may be performed to identify any intracranial abnormalities.
Treatment of Papilledema
The treatment of papilledema focuses on addressing the underlying condition causing increased intracranial pressure. Management options may include:
- Medication: Diuretics may be prescribed to reduce cerebrospinal fluid production and alleviate pressure on the optic nerve.
- Surgical Intervention: In cases of space-occupying lesions or conditions like hydrocephalus, surgical procedures may be necessary to relieve pressure.
- Lifestyle Modifications: Patients with idiopathic intracranial hypertension may benefit from weight loss and lifestyle changes.
- Regular Monitoring: Close monitoring of visual function and optic disc swelling is essential to assess treatment effectiveness.
2. Optic Nerve Disorders
Individuals with preexisting optic nerve disorders, such as glaucoma, are at an increased risk of experiencing TVL.
These episodes may be due to transient ischemia or increased intraocular pressure. Optic nerve disorders encompass a range of conditions that affect the optic nerve, a vital pathway for visual information.
Glaucoma, optic neuritis, ischemic optic neuropathy, optic nerve atrophy, and papilledema are common examples. These disorders can lead to vision impairment and even blindness. Early detection and prompt medical intervention are crucial for effective management.
3. Hypotension
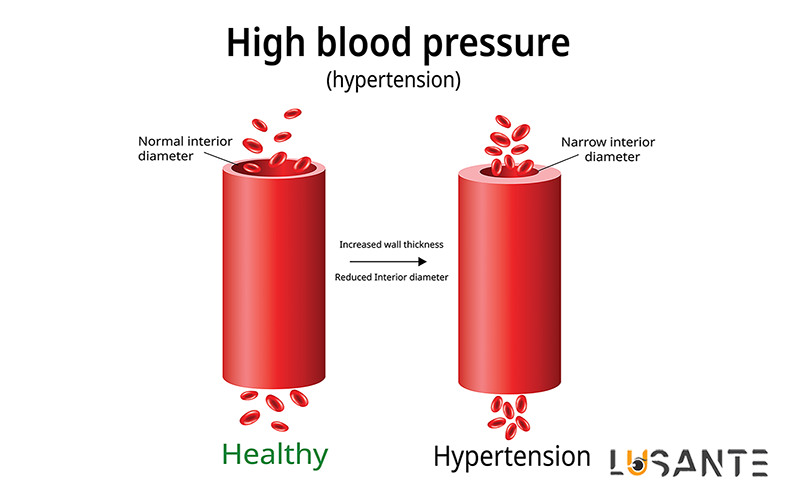
Transient vision loss can occur in cases of severe hypotension or orthostatic hypotension. Changes in blood pressure, particularly when rising from a seated or lying position, can result in decreased blood flow to the optic nerve.
Hypotension, or low blood pressure, is a condition characterized by an abnormally low pressure in the circulatory system. It can lead to symptoms such as dizziness, fainting, and fatigue. While some people have naturally low blood pressure, severe hypotension can be a sign of an underlying health issue and should be evaluated by a healthcare professional.
Lifestyle changes, medication, or treatment of the underlying cause may be necessary to manage hypotension and prevent complications.
Ralated Article: How to prevent hypertension-related ocular complications?
4. Migraines
Migraine headaches are known to cause various visual disturbances, including TVL. Migraine-induced TVL typically involves temporary visual obscurations associated with scotomas or flickering lights. Patients with a history of migraines are at an increased risk.
Migraines are debilitating headaches often accompanied by pulsating pain, nausea, and sensitivity to light and sound. They can significantly disrupt daily life. Migraines may be triggered by various factors, including stress, certain foods, hormonal changes, and more.
While there is no cure, management strategies like lifestyle modifications and medications can help reduce the frequency and severity of migraine attacks, improving the quality of life for those who suffer from them.
Ralated Article: Peripheral Vision Loss and Tunnel Vision
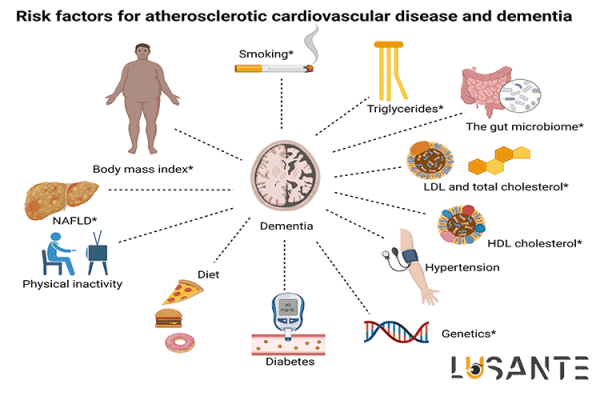
5. Atherosclerosis and Cardiovascular Risk Factors
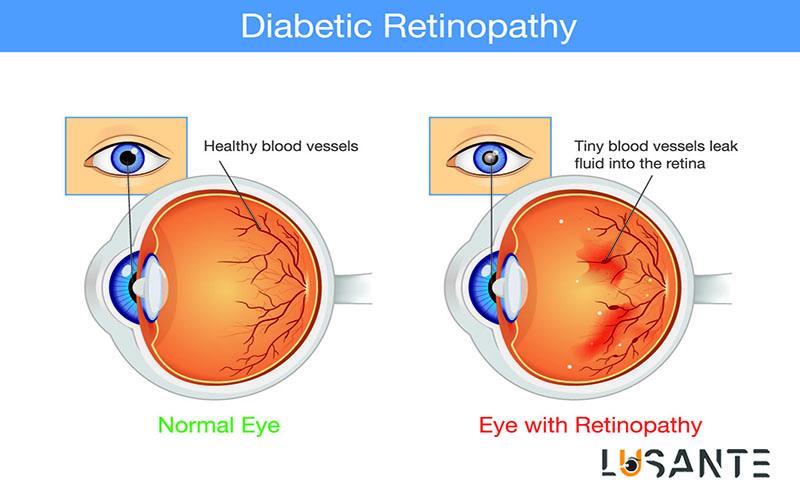
Conditions such as atherosclerosis, hypertension, and diabetes can lead to compromised blood flow to the eye, increasing the risk of transient vision loss.
Atherosclerosis is a progressive disease where fatty deposits accumulate in the arteries, leading to reduced blood flow and an increased risk of heart disease and strokes. Major cardiovascular risk factors include high cholesterol, hypertension, smoking, obesity, and diabetes.
Addressing these risk factors through a healthy lifestyle and, when necessary, medical intervention is vital in preventing and managing atherosclerosis, ultimately reducing the risk of heart-related problems.
6. Medication Side Effects
Some medications have side effects that can lead to TVL. Patients taking medications known to affect blood pressure, blood viscosity, or ocular perfusion may be at risk.
Medication side effects are unintended reactions or symptoms that result from taking a particular drug. These can range from mild, like drowsiness or upset stomach, to severe, such as allergic reactions.
It’s essential for patients to be aware of potential side effects, communicate with healthcare providers, and follow prescribed dosages and instructions to minimize risks and maximize the benefits of their medications.
7. Vasculitis
Inflammatory conditions affecting blood vessels, such as giant cell arteritis, can lead to transient vision loss due to impaired blood flow in the ophthalmic artery.
Vasculitis is a group of rare diseases characterized by inflammation of blood vessels. It can affect vessels of any size, from small capillaries to large arteries. Symptoms vary based on the vessels involved and can range from skin rashes and fatigue to more severe complications like organ damage.
Early diagnosis and appropriate treatment, often involving immunosuppressive medications, are crucial in managing vasculitis and preventing long-term damage.
8. Ocular Ischemic Syndrome
This is a rare condition characterized by severe carotid artery stenosis and ocular hypoperfusion. TVL can be one of the presenting symptoms in these cases.
Ocular Ischemic Syndrome is a rare condition characterized by severely restricted blood flow to the eye. Typically resulting from carotid artery stenosis, it can lead to vision impairment and, if untreated, even blindness.
Management often involves addressing the underlying vascular issues and may require surgical intervention to restore proper blood flow to the eye, emphasizing the importance of early diagnosis and treatment.
9. Systemic Diseases
Various systemic diseases, including lupus, sarcoidosis, and multiple sclerosis, may manifest with transient vision loss as a neurological or inflammatory complication.
Systemic diseases are medical conditions that affect multiple organ systems in the body. These disorders, such as lupus, sarcoidosis, and multiple sclerosis, can manifest with a wide range of symptoms, making them complex to diagnose and manage.
Treatment often requires a multidisciplinary approach, and early intervention is essential to prevent further complications and improve patients’ quality of life.
10. Ocular Conditions
Individuals with ocular conditions such as retinal artery or vein occlusions, or anterior ischemic optic neuropathy, are at an increased risk of experiencing TVL.
Ocular conditions encompass a diverse array of eye disorders, from common issues like myopia and cataracts to more complex problems such as glaucoma and retinal diseases.
These conditions can affect vision and overall eye health. Regular eye check-ups are vital for early detection and treatment to maintain optimal eye function and prevent complications.