Retinal Vascular Disorders
Retinal Vascular Disorders
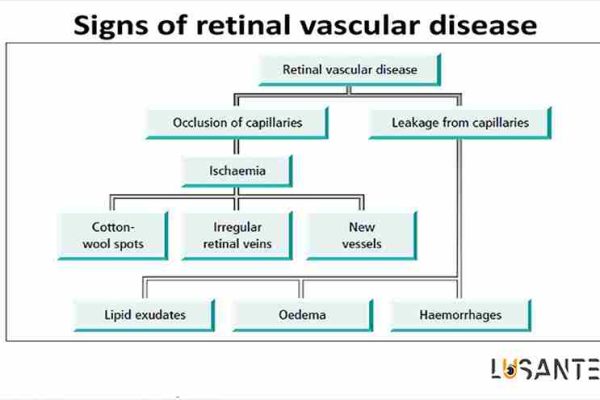
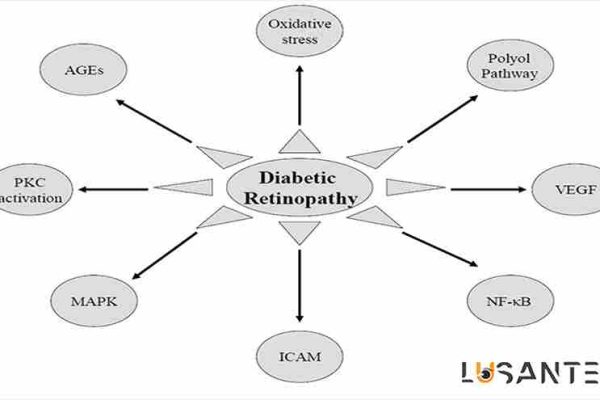
Retinal vascular disorders refer to a variety of retinal disorders such as diabetic retinopathy, hypertensive retinopathy, and retinal vein occlusions; of which diabetic retinopathy is the leading cause of permanent blindness in adults. High blood sugar in diabetics damages the retinal vessel walls and consequently leads to microvascular occlusion, ischemia, retinal hemorrhages, and macular edema. These complications may result in significant vision loss in diabetics. Based on the severity of the disease, there are several treatment options for diabetic retinopathy such as laser photocoagulation, anti-vascular endothelial growth factor intravitreal injections, and vitreoretinal surgery. On the other hand, tight systemic control of blood sugar, lipids, and blood pressure are the mainstay of preventive approaches to diabetic retinopathy, and also help to optimize the effects of treatment.
Oral supplementation may hold promise for controlling diabetes complications via providing antioxidants, and minerals or vitamins which are necessary for microvascular health.
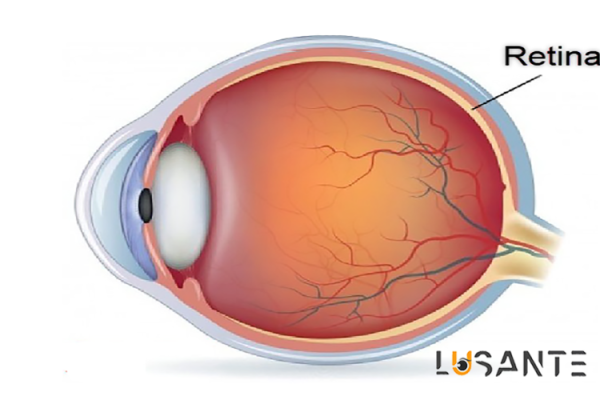
The Retina
The retina is a light-sensitive nerve tissue that is placed as a thin layer inside the posterior part of the eyeball and converts light into nerve messages and sends them to the brain. Therefore, the retina plays a key role in the vision process.
The retina is nourished by a surface layer called the choroid, which surrounds the retina. The rupture of the choroidal retinal structures is associated with retinal hemorrhage and eventually vision loss.
What is Retinal Vascular occlusion?
Retinal Vascular Disorders
The retina is a layer of light-sensitive tissue that covers the back of your eye. It is lined with special cells called rods and cones that convert light into nerve signals and send these signals to the brain so you can see. The retina is a vital part of your vision.
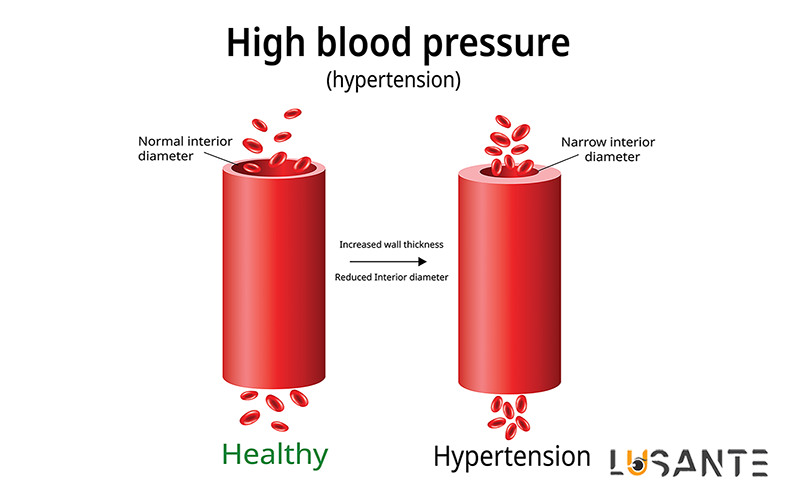
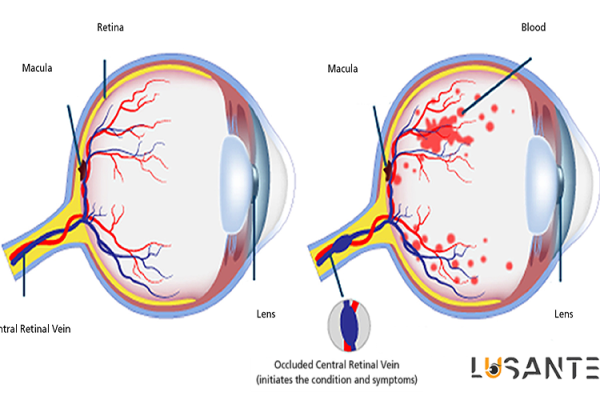
The vascular system consists of blood vessels called arteries and veins that carry blood throughout your body, including your eyes. Your retina needs a constant supply of oxygenated blood that is provided by blood vessels. The blockage of one of these vessels is called Vascular occlusion. This occlusion prevents the retina form passing light through and this light blockage causes vision loss. The severity of vision loss may depend on the location of the blockage or clot. It is more likely to occur in in middle-aged and elderly people or people with diabetes, high blood pressure, high cholesterol levels, or other health problems that affect blood flow.
What are the different types of retinal vessel occlusion?
- Retinal artery occlusion
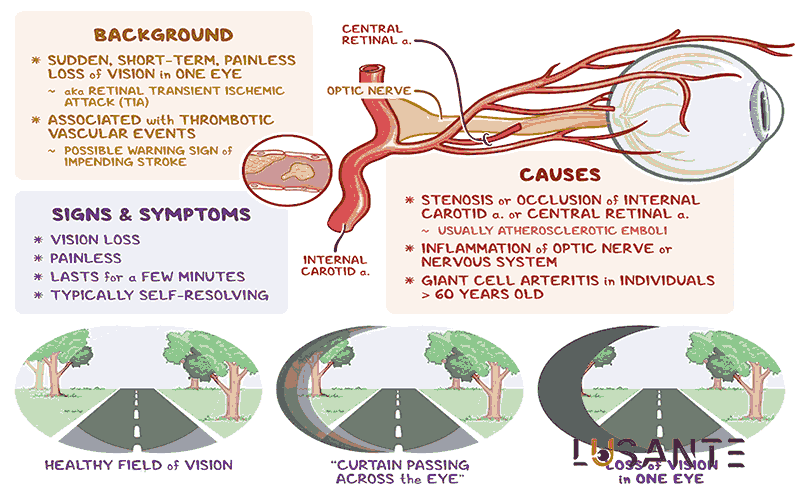
Retinal artery occlusion is blocking of one of the retinal arteries that carry xygenated blood from the heart to the retinal. Central retinal artery occlusion is the blockage of he main retinal artery.
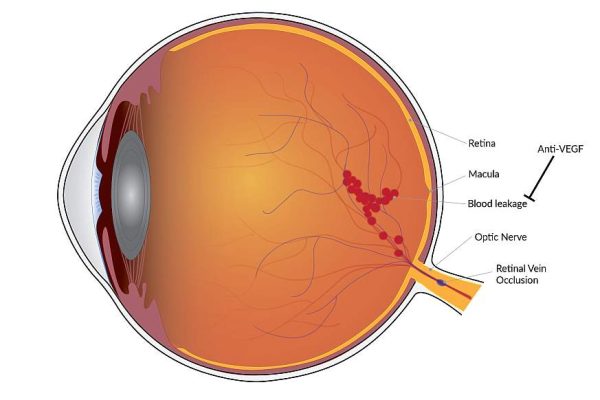
- Retinal vein occlusion
Retinal vein occlusion is blocking of one of the retinal veins that carry deoxygenated blood from the retinal to the heart. Retinal vein occlusion could be divided into two following types:
Central retinal vein occlusion (CRVO) is the occlusion of the main retinal vein.
Branch retinal vein occlusion (BRVO) is the occlusion of branches of the retinal vein.
Central retinal vein occlusion is often more serious than branch retinal vein occlusion.
Causes of retinal vessel occlusion
The certain cause of Retinal Vascular occlusion is unknown. It may happene because the veins in the eye are too narrow. However, there are other factors that affect blood flow and increase the risk of retinal vessel occlusion. These risk factors include:
- Atherosclerosis or hardening of the arteries
- Blood clots, which often appear from other parts of the body
- Blockage or narrowing of the carotid arteries in the neck
- Heart problems, including irregular rhythms or valve problems
- diabetes
- high blood pressure
- high cholesterol
- being overweight
- Intravenous (IV) drug use.
- Being over 60 years old
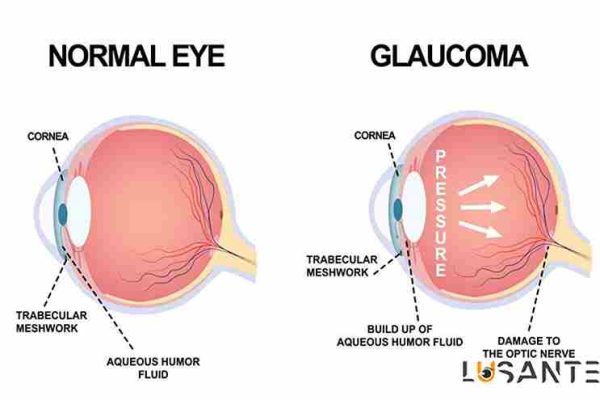
- Glaucoma, which is a condition that damages your optic nerve
- smoking
- Rare blood disorders
- Macular edema, which is fluid accumulation, swelling, and thickening of the central part of the retina.
- Inflammatory disorders such as giant cell arthritis
Symptoms of retinal vessel occlusion
The primary symptom of retinal vessel occlusion is a sudden change in vision. This can include blurred vision, or partial or complete loss of vision. Visual symptoms usually appear in only one eye. Physical pain is not a sign of retinal vessel occlusion. Changes in vision can be temporary or permanent, depending on how quickly you seek treatment and whether you have other health conditions.
Complications of retinal vessel occlusion
This condition can sometimes lead to more serious complications and symptoms. Vision may be severely and permanently affected if any of the following complications occur:
- Macular edema is swelling in the macula, or central part of your retina, due to a buildup of blood.
- Neovascularization is the abnormal growth of blood vessels caused by poor blood flow and lack of oxygen in the retina.
- Neovascular glaucoma involves a build-up of fluid and high pressure in your eye. This is a serious complication. It is associated with severe vision loss and possibly eye loss.
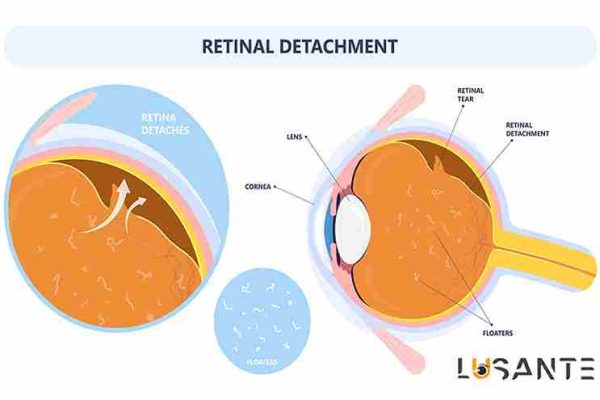
- Retinal detachment is rare. This is the separation of the retina from the contexture of your eye.
Diagnosis of retinal vessel occlusion
Your ophthalmologist will perform a comprehensive examination to diagnose retinal vessel occlusion. They will check your vision, intraocular pressure, and the physical appearance of your eyes. Your doctor will evaluate the function of your eyes and the appearance of your pupils. They may also measure your blood pressure and suggest blood tests to check for blood clotting conditions.
The following eye tests may also be performed:
- Optical coherence tomography (OCT) can be used to take high-quality images of the retina.
- A tool called an ophthalmoscope can be used to examine the retina.
- In a fluorescein angiogram, dye is injected into a special vein in your arm. This vein is the same vein that goes to the blood vessels of the retina. Your doctor can use this to see what happens when the dye is in your eye.
If your doctor suspects that the blood clot is coming from somewhere else in your body, he may suggest other heart tests. These tests may include an echocardiogram, an electrocardiogram, and a heart monitor to check your heart rhythm. These tests evaluate your heart and vascular system.
Prevent retinal vessel occlusion
The best way to prevent retinal vessel occlusion is to identify and treat risk factors. Because retinal vein occlusions are caused by vascular problems, lifestyle and dietary changes are important to protect blood vessels and maintain heart health. These changes include:
- Exercise
- Lose weight or maintain a healthy weight
- Eat a healthy diet low in saturated fat
- Do not smoke or quit smoking
- Control diabetes by maintaining blood sugar at a healthy level
- Taking aspirin or other blood thinners after consulting a doctor
Routine checkups with your doctor can help you find out if you have any of the risk factors for retinal vein occlusion. For example, if your doctor discovers that you have high blood pressure or diabetes, you can start preventive treatment right away.
Retinal vascular diseases
In the following, a number of the most common vascular diseases of the retina are introduced along with their symptoms, complications, diagnosis and treatment.
-
Retinopathy
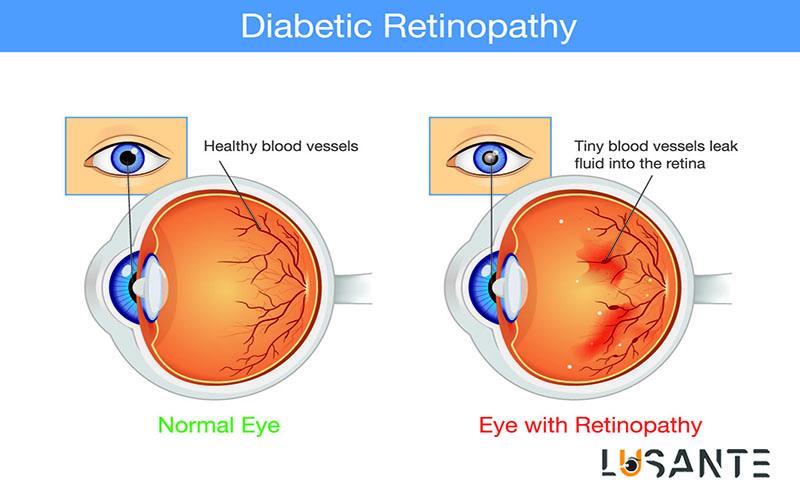
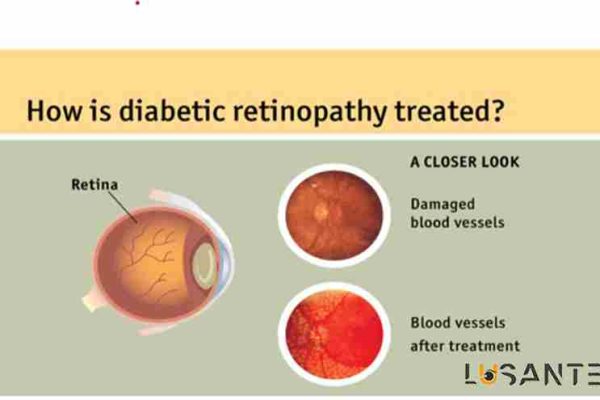
Diabetic retinopathy is a complication caused by diabetes that occurs due to changes in blood vessels and affects the eyes. Damage to blood vessels in the light-sensitive part of the back of the eye, namely the retina, causes diabetic retinopathy. At first, diabetic retinopathy has no symptoms or causes only mild eye problems, but eventually it causes blindness.
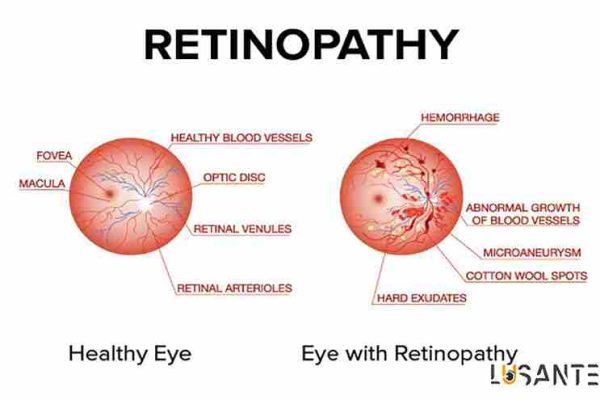
Types of retinopathy
The underlying retinopathy is the first stage: diabetic retinopathy. At this stage, the small vessels in the retina are damaged and fluid or blood leaks from them. The leaked liquid causes swelling of the retina or creates deposits called exudate.
Although this stage usually does not affect vision, it may later progress to more severe stages that lead to vision loss. Therefore, underlying retinopathy is considered as a warning sign. Sometimes the liquid that has leaked collects in the center of vision.
The visual center is responsible for seeing small details of objects (for example, letters or numbers). This is called swelling of the center of vision and may make reading or doing close tasks more difficult.
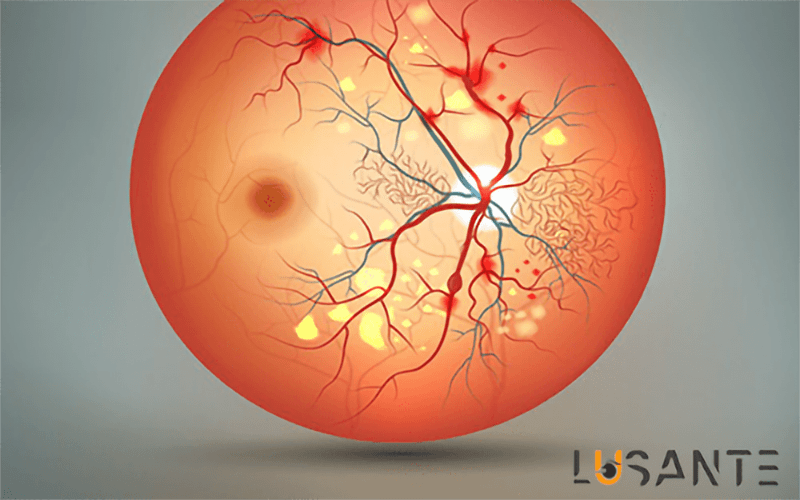
Proliferative retinopathy is a condition in which new and abnormal blood vessels grow on the surface of the retina. This phenomenon is called “Neovascularization”. These new vessels have weaker walls and are fragile and may lead to bleeding.
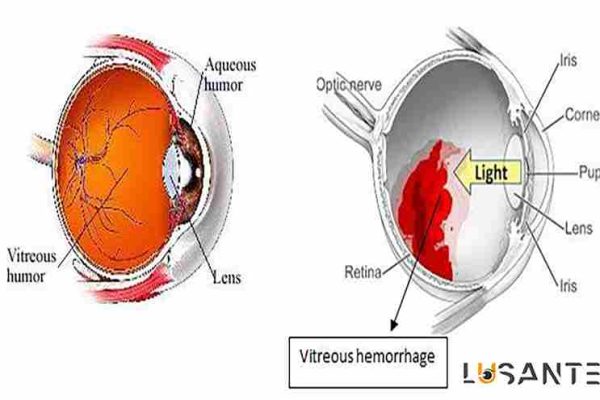
The vitreous is a clear, jelly-like substance that fills the center of the eye. Leaked blood causes the vitreous to become cloudy and partially blocks the passage of light from the pupil to the retina, resulting in a blurred and blurred image.
These abnormal blood vessels may become hardened tissue that separates the retina from the back of the eye and causes retinal detachment, which, if left untreated, can lead to severe vision loss and blindness.
Abnormal blood vessels may also grow around the pupil, on the iris (the colored part of the eye) and cause glaucoma by increasing the pressure inside the eye. Proliferative diabetic retinopathy is the most severe type of retinal disease caused by diabetes. About 20% of diabetics get it.
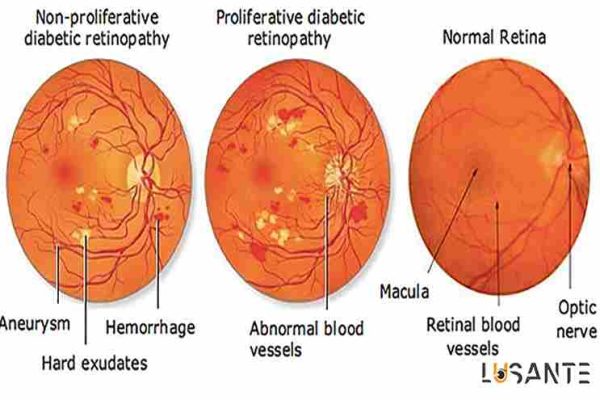
Symptoms of retinopathy
There are usually no symptoms in the underlying retinopathy stage. Although it may gradually develop blurred vision if the center of vision is swollen. You may never notice a change in your vision. Ophthalmological examination is the only way to find the changes inside your eyes.
When bleeding occurs, your vision is blurred, spots are found in it, and your vision may even be completely lost. Although painless, proliferative diabetic retinopathy is a severe form of the disease and requires immediate medical attention. Pregnancy and high blood pressure may aggravate diabetic retinopathy.
Complications of diabetic retinopathy
Diabetic retinopathy causes the growth of abnormal blood vessels in the retina. Therefore, it causes serious problems in your vision, which include:
- Bleeding of the vitreous eye
The vitreous is a clear jelly-like substance that fills the center of the eye. New blood vessels formed in retinopathy may cause bleeding into the vitreous.
If the amount of bleeding is small, you will only see black spots or lines in front of your eyes (eye flies). In severe cases of bleeding, blood fills the vitreous cavity and completely blocks your vision.
A vitreous hemorrhage does not usually cause permanent vision loss by itself. Most of the time, the blood will clear from the eyes within a few weeks or months, and your vision will return to normal, unless the retina is damaged. Eventually, diabetic retinopathy, glaucoma, or both can lead to total vision loss or blindness.
- Detachment of the retina
Abnormal blood vessels that grow as a result of diabetic retinopathy cause scar tissue to form on the retina. This scarred tissue causes the retina to be stretched from the back of the eye and as a result it is detached. This condition causes floating spots in the eye (flicker’s eye), seeing a flash of light in the eye (ocular spark) and a severe decrease in vision.
- Glaucoma or glaucoma
New blood vessels that grow in the eye prevent the normal flow of fluid out of the eye. As a result, the intraocular pressure increases and causes glaucoma. This high pressure causes damage to the optic nerve that carries the seen images from the eye to the brain.
- Blindness
Eventually, diabetic retinopathy, glaucoma, or both can lead to total vision loss or blindness.
Related Article: Vision Loss
Diabetic retinopathy treatment methods
If the yellow spot is damaged by a person with yellow spot, it may be necessary to use a laser for treatment. But ideally, laser therapy is performed in the early stages of the disease and to prevent further damage.
For more severe degrees of the disease, laser treatment or vitrectomy may be needed. These methods are effective in preventing, maintaining or slowing vision loss.
Newer treatments include injecting anti-vascular endothelial growth factor (anti-VEGF) drugs or steroid drugs into the eye.
Surgery to remove vitreous fluid is performed when intraretinal bleeding or retinal tear has occurred, which are rare in the early stages of retinopathy. Vitrectomy is also performed in cases where significant scar tissue has formed.
Current treatments for diabetic retinopathy are often very effective in preventing, delaying, or slowing vision loss, but they cannot completely cure the disease.
People who are being treated for diabetic retinopathy should be examined by an ophthalmologist regularly to check for any new changes in the eyes. Most people need to renew the treatment as the disease progresses.
Also, in this condition, blood sugar level control is very important. This is true even if you are being treated for retinopathy and your vision has improved. In fact, proper control of blood sugar can help prevent the development of retinopathy.
Diabetic people should be examined by an ophthalmologist as soon as possible if they have any signs of retinopathy.
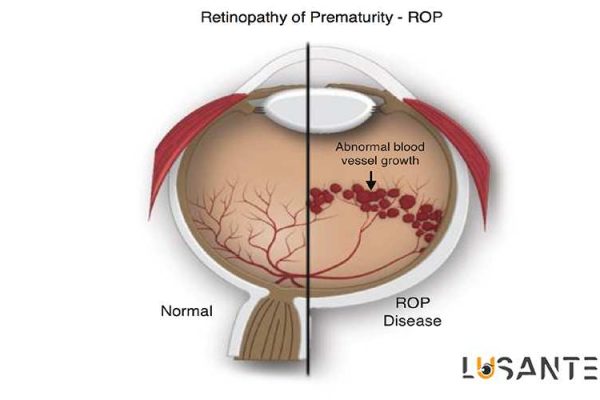
Retinopathy (retinal problems) in premature babies
Retinopathy (retinal problems) in premature babies (Retinopathy of Prematurity – ROP), which is also called Retrolental Fibroplasia, can cause blindness.
In the past, this disease was caused by the use of large amounts of oxygen in the devices in which premature babies were kept, but today, with the progress in the methods of keeping premature babies, the incidence of this disease has decreased.
Factors that put the baby at a higher risk of developing retinopathy are low birth weight (less than 1.5 kg) and premature delivery (26 to 28 weeks).
In premature children, the growth and development of retinal blood vessels have problems and abnormal blood vessels begin to grow. The problem with the growth of abnormal blood vessels, which is also called neovascularization, is that they do not provide enough oxygen to the retina.
Retinopathy in premature babies is divided into 5 degrees depending on the severity of the disease. Progression of the disease to the last degree can cause retinal ulcers and complications such as retinal detachment, vitreous bleeding, eye deviation, and eye laziness. Many babies with retinopathy will develop nearsightedness.

-
Signs and symptoms of retinopathy in premature babies
Since the baby cannot tell his symptoms, parents, pediatricians and ophthalmologists should be aware of the risk factors that increase the possibility of contracting this disease. These factors include:
- Low birth weight (1.5 kg or less)
- Oxygen requirement in the first week after birth
- Having a problem with the baby’s health immediately after birth
Children who have been diagnosed with this disease in infancy should be considered for the following symptoms that may be signs of infection:
- Keeping objects close to the eyes
- Difficulty seeing far away
- Closing and narrowing of the neck of one eye
- Reluctance to use one eye
- Poor vision (not previously diagnosed by a doctor)
- Sudden loss of vision
- eye deviation
-
Diagnosis and treatment of retinopathy in premature babies
Babies who are at risk of ROP should have an eye exam at 4 to 6 weeks after birth. The ophthalmologist first opens the pupil using dilating drops and then sees the retina using an ophthalmoscope.
During the examination, the father or mother must hold the child. Regardless of whether the patient needs treatment or not, he should be re-examined at the intervals specified by the ophthalmologist.
Periodic examinations are necessary to determine whether the disease has stopped progressing and whether treatment is needed.
Some children with grade 1 or 2 disease recover without treatment. In other cases, treatment is necessary if the patient shows symptoms of grade 3 or higher. To prevent the spread of abnormal blood vessels, areas of the retina may be treated with a procedure called cryotherapy.
In this method, parts of the retina are frozen. Laser may also be used for this purpose. In both methods, permanent scars remain in the peripheral parts of the retina, but in most cases, these treatment methods are successful in preserving the patient’s central vision.
-
Macular degeneration
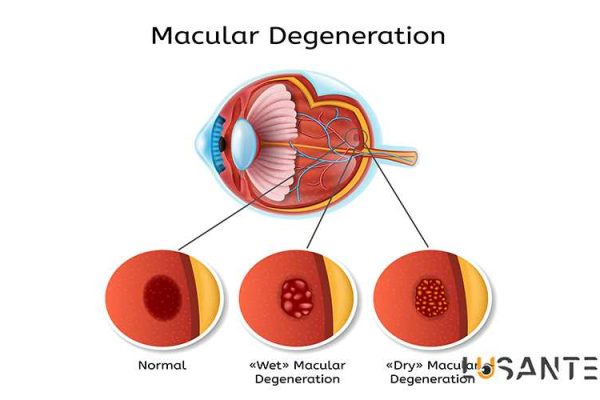
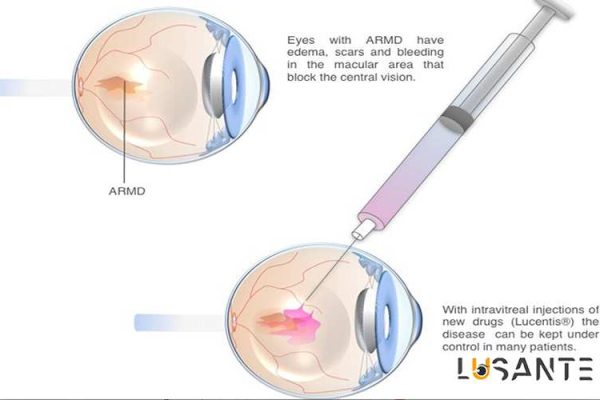
Macular degeneration (AMD or ARMD) is the most common cause of blindness in the world! In this disease, the macula or yellow spot is destroyed.
The macula is the light-sensitive part of the retina and is responsible for direct and clear vision, which is necessary for precise tasks such as reading and driving.
Related Article: 8 Amazing ways to Prevent Age-Related Macular Degeneration
A
There are two types of macular degeneration: Dry and Wet. Dry type is more common and about 90% of patients are affected by this type. The wet type is usually associated with more severe and serious vision loss.
Macular degeneration is more common in people over 65 years old and women are more affected by this disease. Most cases of this disease occur with age. This disease can also be a complication of some drugs. It also seems that inheritance also plays a role in contracting this disease.
-
Signs and symptoms of macular degeneration
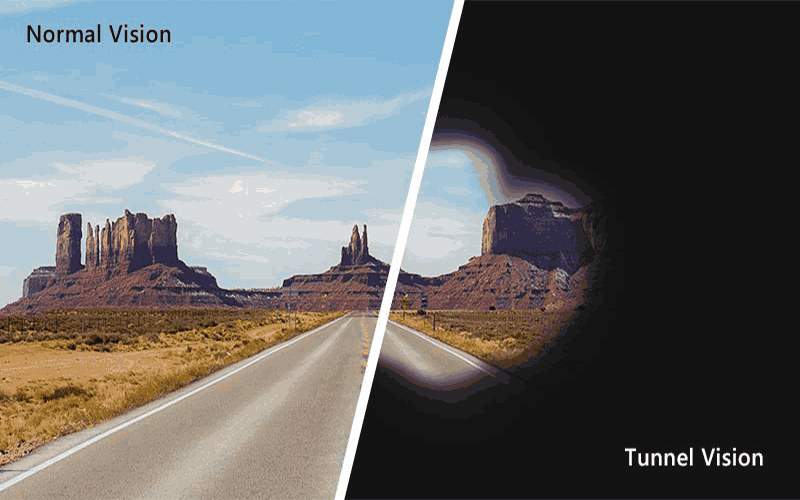
Macular degeneration can cause gradual or sudden loss of vision. If you see wavy straight lines, blurry vision, or dark spots in the center of your vision, you may have early signs of macular degeneration.
In many cases, before the patient has symptoms, the ophthalmologist detects the initial symptoms of the disease during the examination. This is usually done through a visual field test.
In macular degeneration, the central vision is disturbed and the patient sees a black spot in the center of his vision.
Causes of macular degeneration
The exact cause of this disease is not yet known. The dry type may be caused by aging and thinning of the macular tissue, deposition of pigments in the macula, or a combination of the two.
In the wet type, new blood vessels grow under the retina and blood and fluid leak from them. This leakage causes retinal cells to die and causes blind spots in central vision.
Factors that increase the chance of developing the disease include: family history, smoking, high blood pressure, myopia and obesity.
Many researchers and ophthalmologists believe that some foods such as zinc, lutein, xyxantine and vitamins A, C and E help reduce the risk of developing the disease or slow down the progression of dry AMD. Fats may also play a role.
In a study whose results were published in the August 2001 issue of the ophthalmology journal Archive of Ophthalmology, it was concluded that the consumption of omega-3 fatty acids, which are found in abundance in fish, has a protective effect against macular degeneration.
On the other hand, consumption of omega-6 fatty acids found in vegetable oils increases the risk. Some cases of macular degeneration are a complication of toxic drugs such as chloroquine (an antimalarial drug) or phenothiazines (a class of psychiatric drugs).
Treatment of macular degeneration
There is no definitive cure for this disease, but there are treatments to prevent the patient from progressing or even improve vision.
Vitamins and minerals: Research has shown that antioxidant vitamins such as beta-carotene (vitamin A) and vitamins C and E may protect the macula from damage. Recently, in a study on 3600 patients, it has been shown that the consumption of vitamins C, E, beta-carotene and zinc reduces the risk of disease progression in some patients by 28%. These findings lead the researchers to advise patients at risk of advanced AMD to consume antioxidants and zinc in the following amounts. The recommended values are as follows:
- 500 mg of vitamin C
- 400 units of vitamin E
- 15 mg of beta-carotene
- 80 mg of zinc oxide
It should be noted that those who smoke should not use beta-carotene pills because the risk of lung cancer in these people and those who have just quit smoking increases with beta-carotene consumption.
Drug treatment with Visudyne: Visudyne is the first drug used for wet type. In this treatment method, the medicine is injected into the patient’s hand and then it is activated using a non-thermal laser. The activation of the drug causes a chemical reaction that destroys the abnormal blood vessels. 1 out of 6 treated patients get better vision and this is twice as much as patients who do not use this drug.
Laser treatment: Laser photocoagulation improves patients with wet type by destroying and insulating new blood vessels and preventing blood and fluid leakage. In this method, a laser scar remains on the retina and causes blind spots in the patient’s vision. Researchers are investigating ways to reduce the scars and also treat the dry type of the disease with laser.
Blood Filtration: In this method, which was invented by the Japanese about 2 decades ago, the different flow of blood in the membrane reduces the amount of some proteins and fatty acids that are high and may be harmful. This technique has been used in various diseases, but a new type called Rheopheresis has been tested for the treatment of dry AMD. Rheopheresis has not yet been approved by the US Food and Drug Administration (FDA), but is commercially available in Canada and Europe.
Implantable Telescope: This is a small telescopic device that magnifies the image and puts it on the retina. Enlarging the image causes the ratio of the destroyed part of the macula to decrease to the size of the image, and as a result, the spots seen in the central vision become smaller. The Implantable Miniature Telescope was invented in the late 1990s and has now been tested on 200 patients.
Devices used to reduce vision: Although recent advances have been made in the treatment of AMD, lost vision cannot be reversed. For patients who have lost their vision, there are devices that help improve vision by using magnifying lenses and high light. Some of these devices transfer the image to the more peripheral parts of the retina and outside of the macula.
-
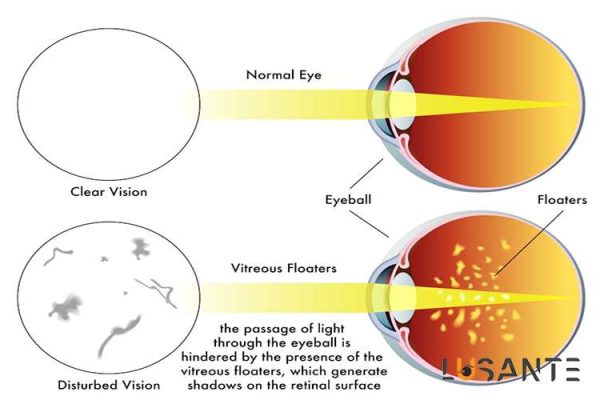
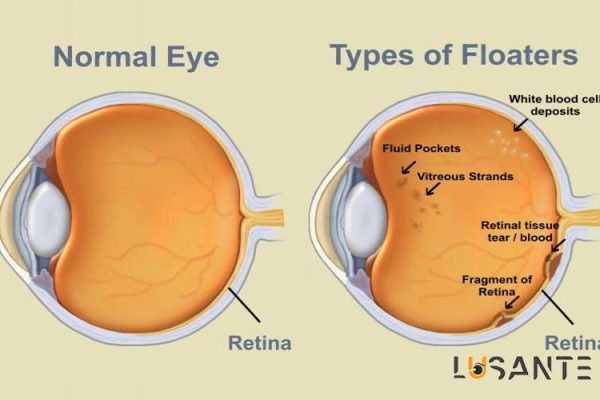
Floaters and Flashes
Have you ever noticed tiny dust particles moving up and down in front of your eyes when you stare at a flat background like a white paper or blue sky?
They remain visible as you blink and they look like cobwebs, worms, rings, dots, or specks. These disturbing shadows are called Floaters. Usually, Floaters appear by eye movement, but they are vague and unclear because they float in the opposite direction of the eye movement.
Flashes are sparks of light like camera flashes that flicker in front of the eye. They occur when the vitreous fluid pulls or tugs against the retina.
Floaters are shadows on the retina that are caused by the shrinkage of the vitreous fluid. The turbidity of the vitreous fluid leads to shadows on the retina which are seen as dark shadows.
These turbidities may be caused by the adhesion and stickiness of the vitreous fibers, accumulation of inflammatory cells in the vitreous, or bleeding inside the eye.
What is vitreous?
The vitreous is a jelly-like liquid similar to raw egg white that fills most of the inside of the eyeball (from behind the lens to the retina) and helps maintain the spherical structure of the eye and keeps the retina in place.
The structure of the vitreous is created from a spongy network consisting of very fine filaments, which contain large amounts of water and soluble substances and gives it a jelly-like state.
The filaments in the vitreous are denser in the outer parts of the vitreous and have relatively tight connections to the inner layers of the retina.
Common Causes of Floaters and Flashes
Floaters and Flashes are common and harmless complications and their prevalence increases with age. In general, more than 60-70% of people aged over 60 years have experienced Floaters and Flashes.
In children and young people, the vitreous filaments are usually very delicate and transparent, but with aging, these filaments become thicker and stick together in some places, causing opacity, the shadow of which is felt on the retina in the form of floaters and flashes.
In addition, in many elderly people, a part of the peripheral fibers of the vitreous, which is connected to the retina, is torn from its place and falls into the central parts of the vitreous.
This condition, which is called posterior vitreous detachment, is the most common cause of floaters and flashes. Sometimes the presence of intraocular inflammation (uveitis) causes the accumulation of inflammatory cells in the vitreous, which causes floaters and flashes.
Another cause of Floaters and Flashes is bleeding inside the vitreous; For example, in people with diabetes, mild eye bleeding may first be seen as floaters and flashes.
Other causes of floaters and flashes:
- People over 60 years old
- Myopic people
- People who have a history of eye surgery (especially cataract surgery).
- People who have a history of intraocular inflammation (uveitis).